Revolutionizing Menopause with a Breakthrough Treatment Sparks Hope
Menopause, the inevitable reality
One of the inevitable and natural processes that happens to a woman’s body is the onset of menopause. That time can indicate the end of a woman’s menstrual cycle. Typically, if the woman is said to have missed the menstrual period for a continuous 12 months, she is believed to have reached the menopause stage. Conversely, if at least 12 months have passed, since she had her last normal period, she is said to have menopause. There is never a fixed time frame for this condition, but usually, it can happen in women who are in their 40’s and 50’s of age.
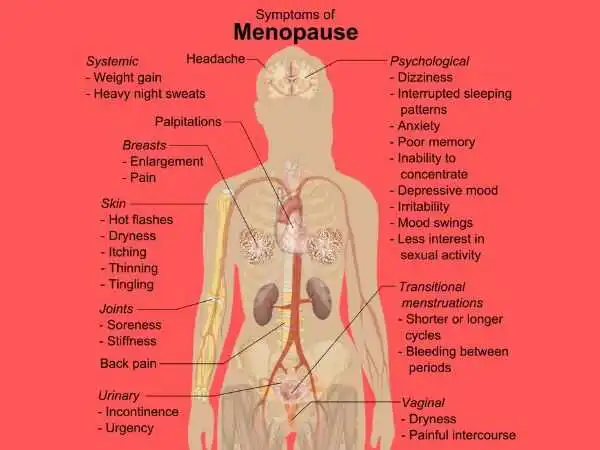
Although this should be treated as a normal condition for every woman and accepted gracefully, the other factors that come with it should be dealt with with maturity and patience. The symptoms like feeling low, getting emotionally drained out, going through hot flashes, feeling sleep disorder, night sweats, mood changes, etc. are the conditions that one should be aware of. Menopause itself is not the problem, but those temporary symptoms that are associated with it are to be negotiated effectively. In short, the side effects of this condition need to be better-taken care of.
The cure is in the making
But the good news is that relief for such women is not too far away now. The scientists from the biotech company Oviva Therapeutics claim to have developed an injection that can effectively delay the onset of menopause itself.
“This drug couldn’t just delay menopause, it could actually prevent it,’ said the molecular biologist from Oviva Therapeutics, Dr. Daisy Robinton, to the ‘Daily Mail’.
During her address in a presentation at Livelong Summit last week, Dr. Robinton talked extensively about her company and its working. Although the company’s menopausal medication and treatment is currently in the mouse trial stage and may take years to reach the market if at all, it did manage to land a $12 million licensing contract with Mass General in 2022.
“The work that we’re doing at Oviva Therapeutics looks to the ovaries as fundamental to our health and well-being,” Dr. Robinton told Pharmacy Times ahead of her talk at the conference in Palm Beach, Florida, “and has the goal of being able to preserve ovarian function for a greater period of time so that we can extend health span for women and make menopause something that can be optional through therapeutic intervention.”

While presenting her research, at the summit, she said, “AMH hormone controls the amount of lag time until the menopause and actually acts as a brake in females,”. We could use AMH to slow the loss of ovarian reserve [number of eggs in the ovaries] and extend the runway to the menopause.”
The drug is in the testing stage
As per Daily Mail, the new medicine, given every few months, is being tested on rodents to make sure it’s safe. If it works well in these tests, it might be tried out on humans in the next few years. But if it does get approved for humans later on, it could cost a lot of money, possibly six figures, because the research to develop it is quite expensive.
Although the researchers didn’t mention any bad effects from the injection, hormone replacement therapy (which boosts estrogen and progesterone in menopausal women to ease symptoms but doesn’t delay menopause) has been linked to higher chances of cancer, blood clots, and stroke.
Dr. Robinton in an interview with the ‘Pharmacy Times’, said, “Our ovaries and a woman’s body are really the seat of health in many ways — the hormones that they produce provide a sort of homeostasis or consistent quality of life during a woman’s reproductive years, if her reproductive organs are functioning sort of in a normal range”
Watch out for the after-effects
It’s not just about long-term fertility, she continued: “We see that once a woman goes through menopause, she has significantly increased risks of cardiovascular disease, very significant declines in neurocognitive health (so many women experienced ‘brain fog’) and there can be increases in anxiety, depression, mood disorders, [and] a lot of sleep dysfunction.”
This research is part of a bigger discussion about how we think about menopause. A group of experts said in a recent article in the Lancet that we shouldn’t see menopause as a problem to be fixed but as a natural part of getting older.
“Even though it’s important to manage symptoms,” they wrote, “seeing menopause as a medical issue can make women feel powerless, leading to too much treatment and ignoring some good things about getting older, like better mental health and not having to deal with periods, period problems, and birth control.”